Editor’s Note
This month’s breakthroughs remind us that innovation thrives at the intersection of persistence and ingenuity.
From decoding SCI’s molecular repair pathways to pioneering salvage microsurgery, uncovering rare infections, and democratizing brain monitoring—each advance pushes neurosurgery’s boundaries. Whether in the lab or OR, curiosity remains our sharpest tool.
— Editor, The Short Report on Neurosurgery
In This Issue
- AI Cracks SCI’s Repair Code :: Breakthrough Targets for Spinal Cord Injury Recovery Identified Using AI & Genetics
- Case Breakthrough : When Thrombectomy Fails, Open Surgery Prevails :: 84yo male walks independently 24h post-op after bicoronal/interhemispheric approach
- Skin Bacterium Invades Pituitary :: The First Adult Case of Primary Pituitary Abscess by Cutibacterium acnes
- Smart, Simple, Surgical: Real-Time Brain Monitoring via RGB Camera :: Real-time Brain Tissue Oxygen Monitoring Using an RGB Camera in Cerebrovascular Surgery
AI Cracks SCI’s Repair Code
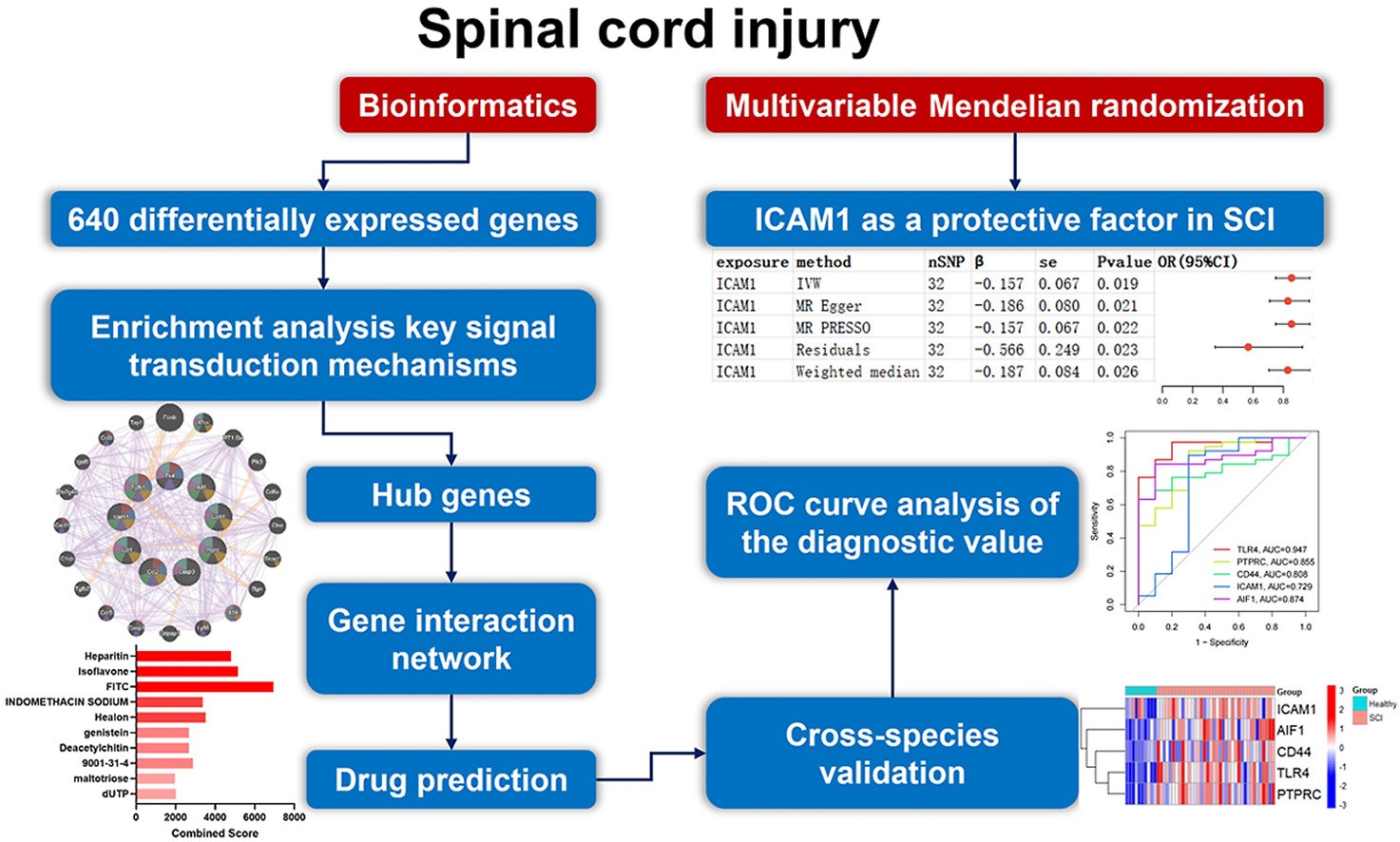
In a groundbreaking study published in World Neurosurgery , researchers have identified key molecular targets and potential drug candidates for repairing subacute spinal cord injuries (SCI)—a critical phase occurring 7 days after trauma.
What They Did: Using a powerful combo of bioinformatics, cross-species transcriptomics, and Mendelian Randomization, the team analyzed over 640 genes from rat, mouse, and human datasets to uncover:
- 5 Diagnostic Biomarkers: TLR4, ICAM1, CD44, PTPRC, and AIF1 — significantly upregulated in SCI and validated across species.
- ICAM1 Found Protective: Using multivariable Mendelian Randomization (MVMR), ICAM1 was shown to have a causal protective effect on SCI, offering a promising therapeutic target.
- Top Drug Candidates: Genistein, dimethyl sulfoxide, and isoflavone—known for modulating inflammation and promoting axonal repair—were identified as top interventions.
Why It Matters: SCI recovery is hindered by inflammation and glial scarring. This study zooms in on the subacute phase—where the body begins its repair—and pinpoints targets that could be modulated to enhance recovery. With high diagnostic accuracy and strong cross-validation, the identified genes and drugs pave the way for precision neuroregenerative therapies.
Case Breakthrough : When Thrombectomy Fails, Open Surgery Prevails
Clinical Challenge
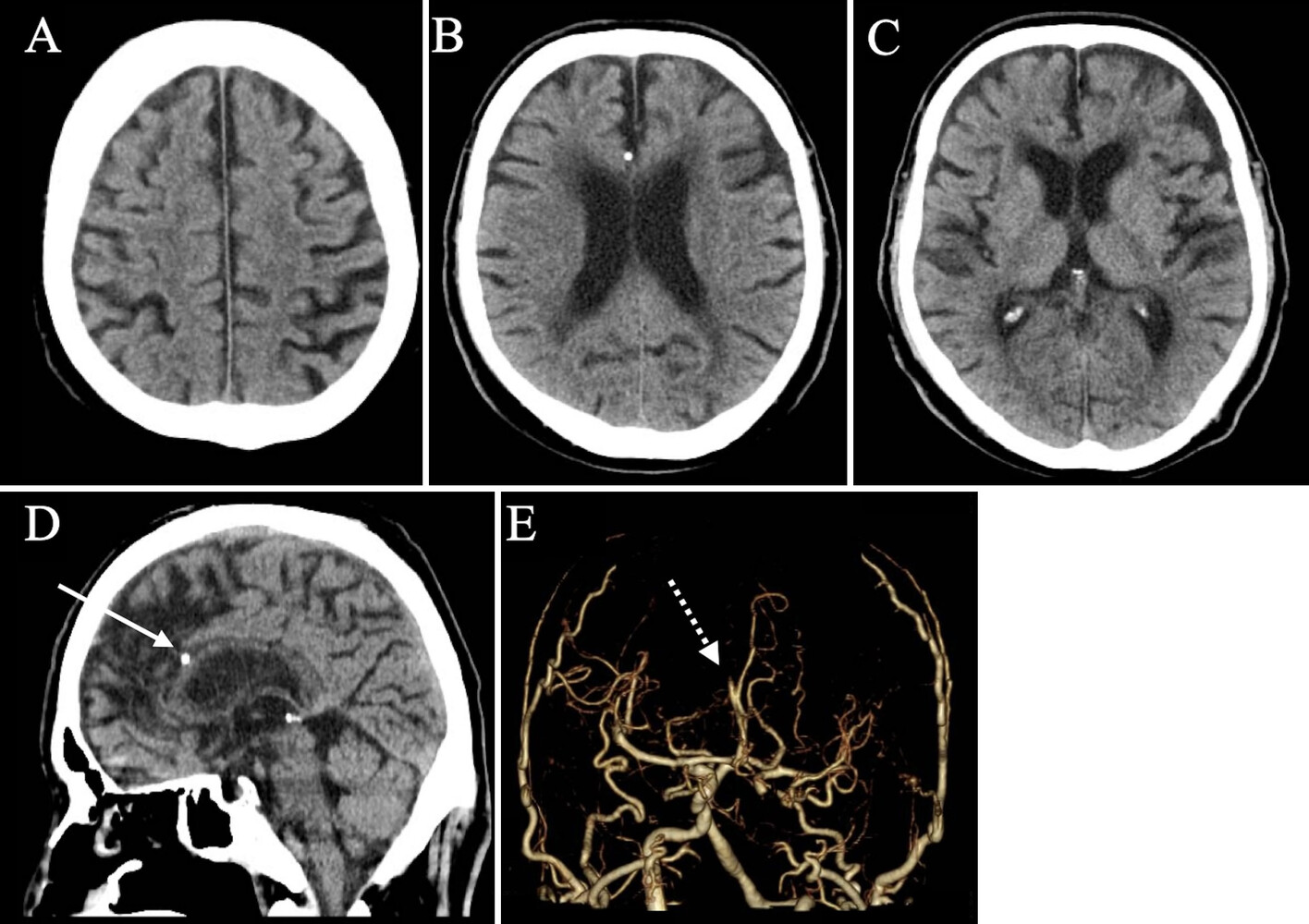
As featured in JNS Case Lessons, an 84-year-old man presented with sudden-onset left lower limb paralysis. Imaging revealed a right anterior cerebral artery (A3) occlusion caused by a severely calcified plaque. Despite IV alteplase and attempted mechanical thrombectomy, revascularization could not be achieved endovascularly.
Surgical Solution
Faced with deteriorating symptoms and a persistent occlusion, the neurosurgical team opted for an emergency endarterectomy via a bicoronal craniotomy and interhemispheric approach. The calcified lesion was surgically removed through a longitudinal arteriotomy. Intraoperative indocyanine green (ICG) angiography confirmed successful flow restoration.
Postoperative Outcome
The patient experienced near-complete recovery of motor function within 24 hours post-op and returned to walking independently. Histology confirmed the presence of calcified plaque with no evidence of active thrombus.
Why it matters
Microsurgical endarterectomy is a viable salvage option when EVT fails, especially for distal ACA occlusions with calcified lesions.
This case is the first documented instance of successful emergency endarterectomy for an A3 occlusion, achieving complete recanalization and favorable outcomes.
Preoperative recognition of calcification on CT should guide early consideration of open surgery.
Technical Insight
Interhemispheric access was preferred due to less tissue disruption and better exposure in elderly patients with brain atrophy.
Longitudinal arteriotomy allowed thorough lesion visualization and safe removal.
⚠️ Intracranial arteries are fragile—careful technique is essential to avoid iatrogenic injury.
Skin Bacterium Invades Pituitary
In a compelling case report published in the Journal of Neurological Surgery Reports, Dr. Chi-Man Yip presents a rare and insightful case of a primary pituitary abscess in a 60-year-old woman caused by the skin bacterium Cutibacterium acnes—marking what is likely the first-ever documented case in an adult.
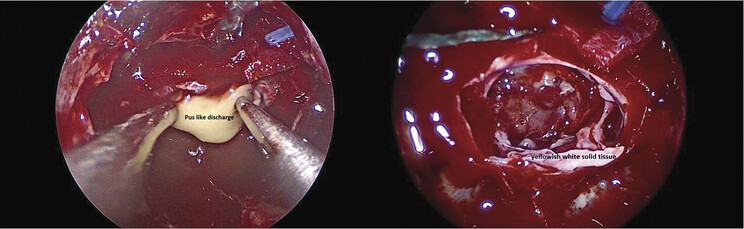
The patient, with a background of diabetes mellitus, reported with fever, headache, and signs of hypopituitarism. Imaging revealed a rim-enhancing sellar mass, initially suspected to be a cystic pituitary adenoma.
Surgical intervention via an endoscopic endonasal transsphenoidal approach revealed pus and solid tissue. Culture identified C. acnes, and histology showed non-neoplastic pituitary tissue with chronic inflammation. Post-surgical recovery was excellent with antibiotic therapy, though hormone replacement continues due to persistent hypopituitarism.
Cutibacterium acnes is commonly found in the skin flora and is rarely pathogenic in the brain. Its role in this case highlights the organism’s potential as an opportunistic pathogen, especially in immunocompromised individuals such as those with diabetes.
Why It Matters:
Diagnostic Challenge: Pituitary abscesses often mimic more common lesions like adenomas and are difficult to diagnose preoperatively.
Microbial Awareness: This case urges clinicians to consider C. acnes in culture-negative abscesses and to be mindful of its underrecognized role in deep infections.
First in Literature: It adds a unique entry to neurosurgical literature by documenting the first adult case of C. acnes-related primary pituitary abscess.
Interdisciplinary Importance: Successful outcome reflects the need for tight collaboration between neurosurgery, infectious diseases, and endocrinology teams.
Smart, Simple, Surgical: Real-Time Brain Monitoring via RGB Camera
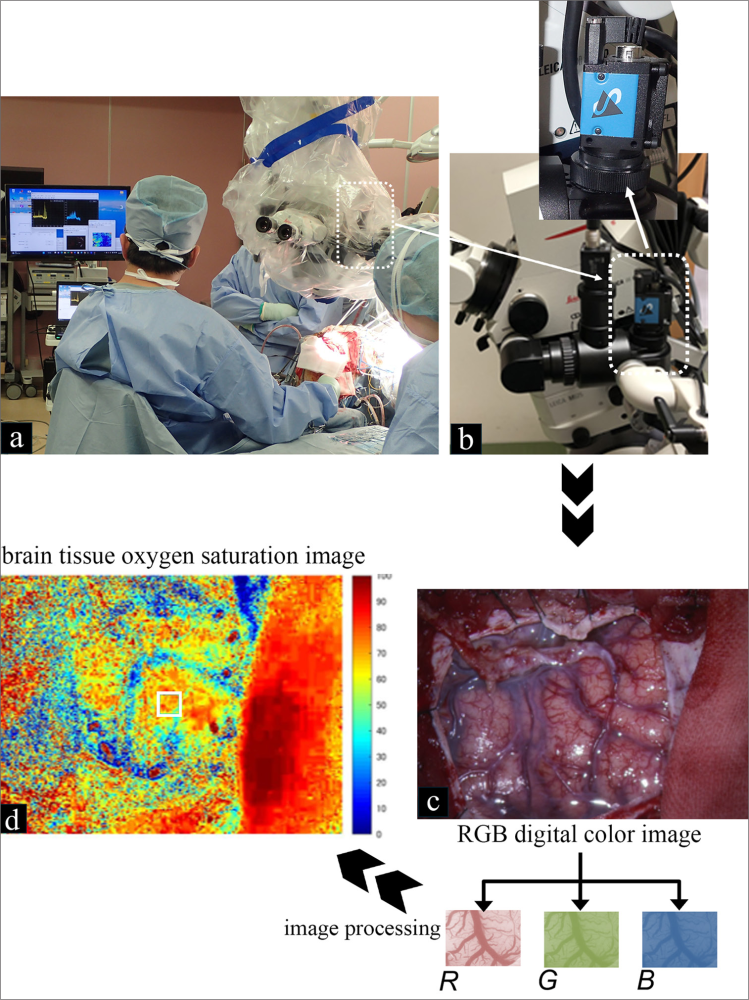
In a promising advance for intraoperative safety, researchers from Yamagata University and Tokyo University of Agriculture and Technology have developed a cost-effective, real-time brain tissue oxygenation monitoring system using a standard red-green-blue (RGB) camera. The technique was validated in a study published in Surgical Neurology International, demonstrating its ability to track brain surface oxygen saturation (StO₂) during cerebrovascular surgeries like Moyamoya bypass and aneurysm clipping.
The RGB camera—adapted to standard surgical microscopes—enabled continuous, non-contact monitoring, highlighting oxygenation changes that correlated with critical outcomes such as cerebral hyperperfusion syndrome (CHS) and motor-evoked potential (MEP) decline. Patients with a ΔStO₂ increase >10% were more likely to develop CHS, while sustained StO₂ drops during temporary artery occlusion aligned with MEP deterioration.
Unlike traditional methods (ICG angiography, NIRS, or laser speckle imaging), this RGB-based approach is low-cost, highly versatile, and allows real-time intraoperative decisions, making it especially relevant for neurosurgical teams in both high-resource and resource-limited environments.
Why It Matters: Predicting and preventing intraoperative ischemia or CHS remains a major challenge in neurosurgery. This low-cost, non-invasive technology may become a game-changer in global neurosurgical safety, especially in resource-limited settings. Its compatibility with any surgical microscope and real-time feedback offer tremendous clinical value—helping surgeons make data-informed decisions when stakes are highest.
That’s a wrap on this edition of The Short Report on Neurosurgery!
Which of these advancements intrigued you the most? Let’s discuss in the comments! 💬
🔗 Follow & Subscribe to stay ahead of the latest in neurosurgery.
Leave a comment